Updated January 28, 2025
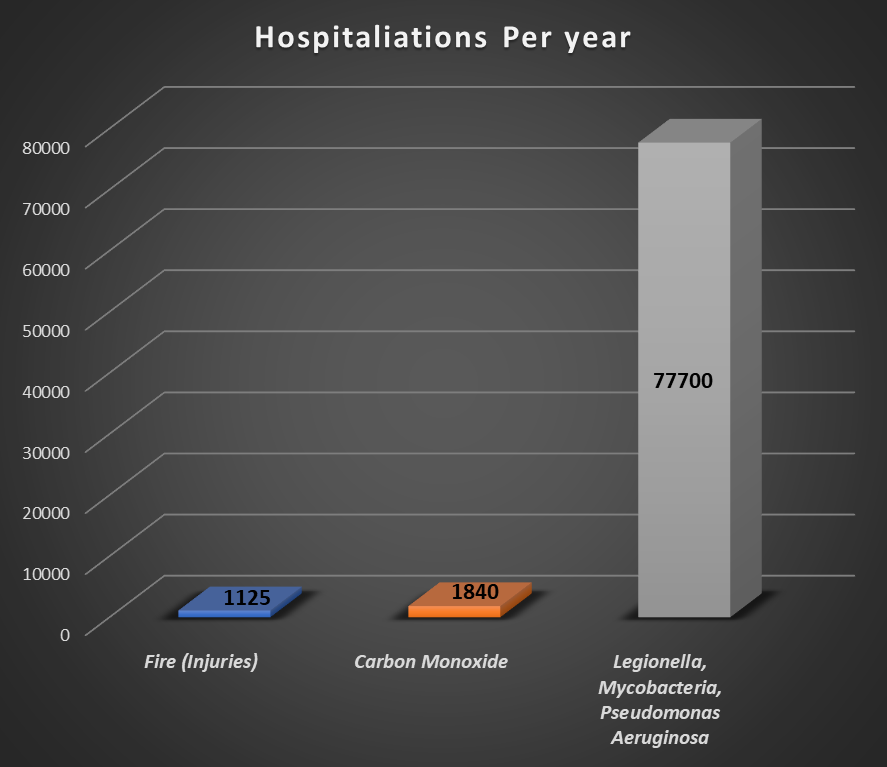
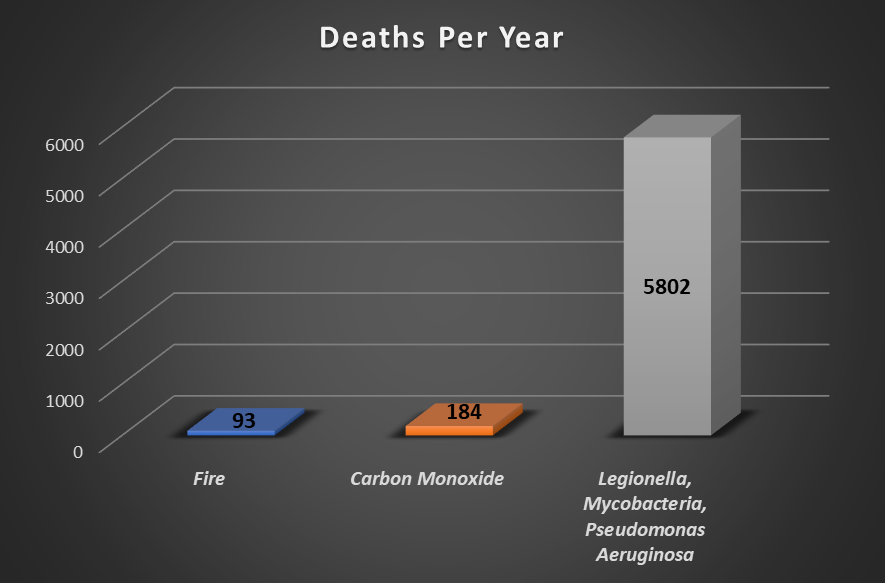
Healthy building initiatives that have in recent years been emphasized in the United States and Europe are important since so many people spend a large part of their lives indoors. What seems out of sync with health data, though, is that the term “healthy building” has focused mostly on air contaminants which, compared with water, cause a relatively small percentage of hospitalizations and deaths (see figures below).
“Healthy building” initiatives have focused on air. Many buildings have sensors installed in ducts to measure particulate matter (PM 2.5), carbon dioxide, carbon monoxide, total volatile organic compounds (TVOC), and humidity. Periodic onsite testing is performed to detect radon, mold, formaldehyde, carbon monoxide, asbestos, and other contaminants. Specifications require minimum air exchange rates, turnover rates for air filtration and humidity must be controlled.
Water, by contrast, is almost an afterthought. Several aspirational documents recommend providing safe water and establishing water management programs to control Legionella and other opportunistic premise plumbing pathogens, but few building owners are required by regulations or insurance carriers to implement such measures, and few do.
Water is processed by municipalities in batches and sent through hundreds or thousands of miles of pipes, creating its own flora and fauna and picking up trace amounts of various contaminants along the journey. When the water enters a building, it finds an environment even more favorable for pathogen growth–smaller pipe sizes with more surface area for biofilm formation, warmer temperatures, and cozy crevices in which to hide from disinfectants–and efficient pathways to people (e.g., faucets, showers, hot tubs). Continued low occupancy after COVID has likely made the problem worse because of water stagnation in underused buildings.
Pathogens are not the only water-related cause of illness in buildings. VOCs from disinfectants and disinfection byproducts can be expelled each time a faucet or shower is opened.
Water-related illness is expensive, too. According to the Centers for Disease Control and Prevention (CDC), the estimated direct healthcare cost of biofilm-associated waterborne pathogens such as nontuberculous mycobacteria, Pseudomonas, and Legionella is $2.39 billion yearly in the United States.
Figure 1. Average hospitalizations from carbon monoxide (1,3) or fire (4) in buildings compared with opportunistic premise plumbing pathogens (2). Note: Air contaminants (e.g.,PM2.5, VOCs, humidity etc.) are typically not a direct cause of hospitalization or death.
Figure 2. Average deaths from carbon monoxide(1,3) or fire (4) in buildings compared with opportunistic premise plumbing pathogens.(2)
Think about how far buildings have come with fire safety. Countless lives have been saved because of codes, regulations, technologies, and inspections. Illness and death from waterborne pathogens can be prevented, too.
Momentum for better building water management is gaining steam. Hospitals and nursing homes are already required by the Centers for Medicare & Medicaid Services (CMS) and the Joint Commission to have water management programs that satisfy ASHRAE Standard 188.
The recently adopted New Jersey regulations require Legionella water management programs in many types of large buildings (e.g., hotels, commercial buildings, apartment and condo towers, industrial facilities) in addition to healthcare facilities. Other states may follow suit.
Everything building owners need to get started is available– technologies, advanced data analytics, training, and water management program software with IoT sensor integration and lab automation. If buildings are managed to control water hazards as well as air hazards, they could become healthy indeed. In addition to protecting health and life, a truly healthy building also protects profits and brand equity by attracting tenants and guests and limiting legal risk.
David Swiderski is the Senior Technical Strategist at HC Info.
References:
- CDC. Carbon Monoxide Poisoning. https://www.cdc.gov/co/faqs.htm
- Collier S, Deng L, Adam E, et al. 2021. Estimate of Burden and Direct Healthcare Cost of Infectious Waterborne Disease in the United States. Emerging Infectious Diseases. https://stacks.cdc.gov/view/cdc/99960/cdc_99960_DS1.pdf
- Sircar K, Clower, J, Shin M, et al. 2015. Carbon monoxide poisoning deaths in the United States, 1999 to 2012. The American Journal of Emergency Medicine 33, 9. https://www.sciencedirect.com/science/article/abs/pii/S0735675715003800
- Nonresidential Building Fire Trends (2010-2019). National Fire Data Center (FEMA). https://www.usfa.fema.gov/downloads/pdf/statistics/fire-estimate-summary-series.pdf

Really interesting analysis, what about Radon and Asbestos?
Thank you for your comments, Francesco! Radon and Asbestos are also part of most Healthy Building initiatives and in most cases seem to be periodically measured during construction in certain areas as referenced in the article.
The term healthy buildings applies only to commercial and institutional buildings where there are no industrial processes involving hazardous biological agents nor intentional sources of infectious and other biological agents that cause disease such as acute care hospitals. Hospitals have made a major error in mixing infected patients with well patients eg surgical patients. The concept of a general hospital is antithetical to infection control.
Stephan thank you for your comments! LAMPS actually has 7 building types and we have a wide range of users in the LAMPS community your point is well taken with Hospitals being an extremely challenging environment to provide infection control and prevention.
From my own personal experience, I know that spending a few days indoors causes me a slight respiratory issue. Whilst an hour in my garden eases the problem. These issues I put down to air pollution inside our home.
From my work, I know that water-related illnesses are much-misunderstood.
The lack of knowledge within the general public is an issue.
Whilst Safety issues around the supply of Gas and Electricity are well documented and well understood but the same cannot be said for Water.
In the UK much of the infrastructure supplying water to buildings and homes is 100+ tears old. Few cases of pneumonia are investigated and it is probable that the true figure for UK legionnaires’ cases could be 10 times that recorded by the health authority.
For my part, I struggle to see how we can easily overcome the lack of knowledge. My biannual Newsletter emailed to many of my clients aims to increase awareness of this issue both locally and internationally. I hope that clients read the letter and. thereby raising the level of awareness of the risks associated with neglecting their water systems.
It is going to be a long hard road.
Peter thank you for your comments and insight on the UK!
Until people(building owners) are required by law or insurance to have a Water Management Program, many will not voluntarily comply. It is an added cost and they don’t see the risk for themselves. I also think the water utility is not doing all they could be doing and in some places not even complying with regulations. Increased disinfection levels and disinfection types should be looked at more closely. Here again, the cost is a factor, and throw in DBPs.
David thank you for your comments! There definitely is quite a bit of opportunity to improve on many fronts. I find it interesting there is little in the way of laws for many of the Healthy Building sensors, testing, and monitoring however, for fire, carbon monoxide, radon, etc. there definitely has been a need for both legislative and insurance policy action.
I completely agree that water has been a long overlooked component of “healthy buildings” with most studies focusing on air quality as the primary element responsible for occupant illness. Water quality is actually a more complex issue than air with each building having a unique “signature” with respect to water composition, flow, and facility structure and water chemistry is constantly in flux. In addition, to health issues, waterborne pathogens have been at the forefront of increasing litigation and insurance claims for property damage, bodily injury and cost of remediation as well as other related costs. While insurance coverage may be available for these types of claims, building owners/managers will often have to demonstrate successful control of waterborne hazards, compliance with ASHRAE 188, and the ability to respond to issues should they occur.
Your comments on legal liability are very helpful which is in addition to lost brand value. You always have been at the forefront of this issue and your insights are very helpful to everyone in the LAMPS community. Russ, thank you very much for your comments and invaluable legal insight!
Fascinating stuff – and so timely! I’ve been working in hospitals for 40+ years and the notion that the healthcare environment can be “measured” just by using square footage falls short of a sense of the whole. While the focus on life safety is always a priority, it’s the focus on how building systems can (and should) support patient care that will drive improvement and increase safety.
Thank you for your comments Steve!